Description
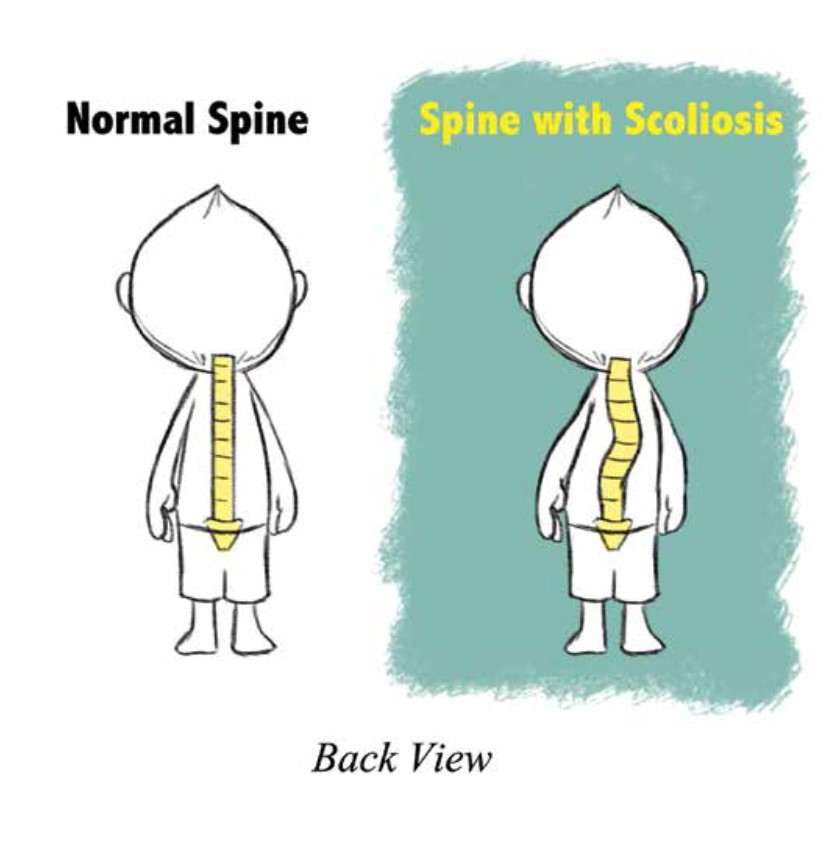
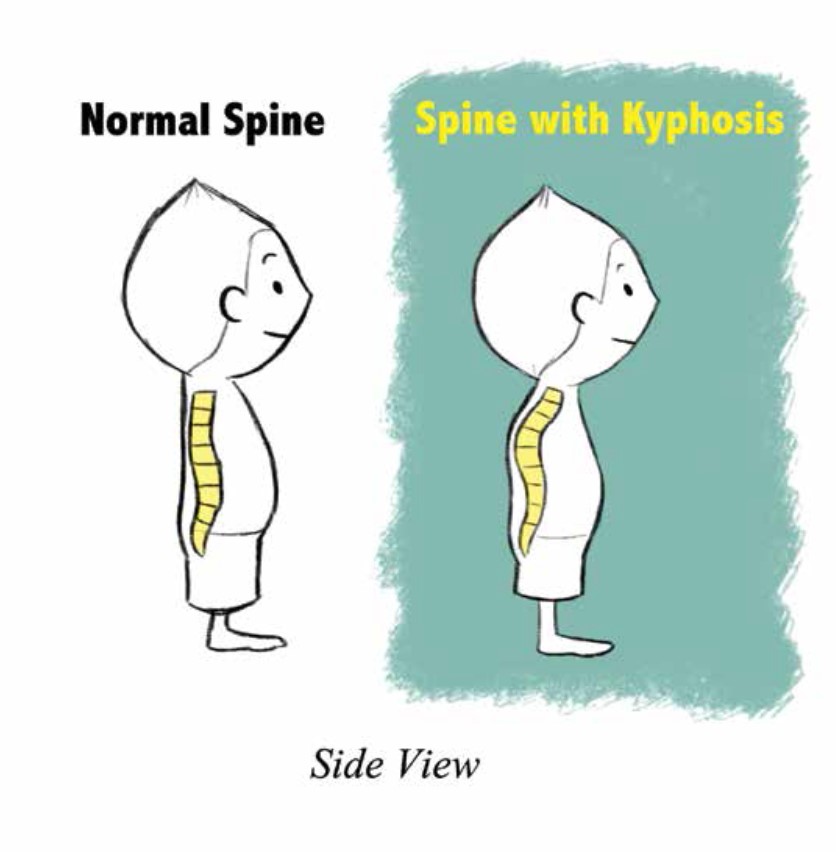
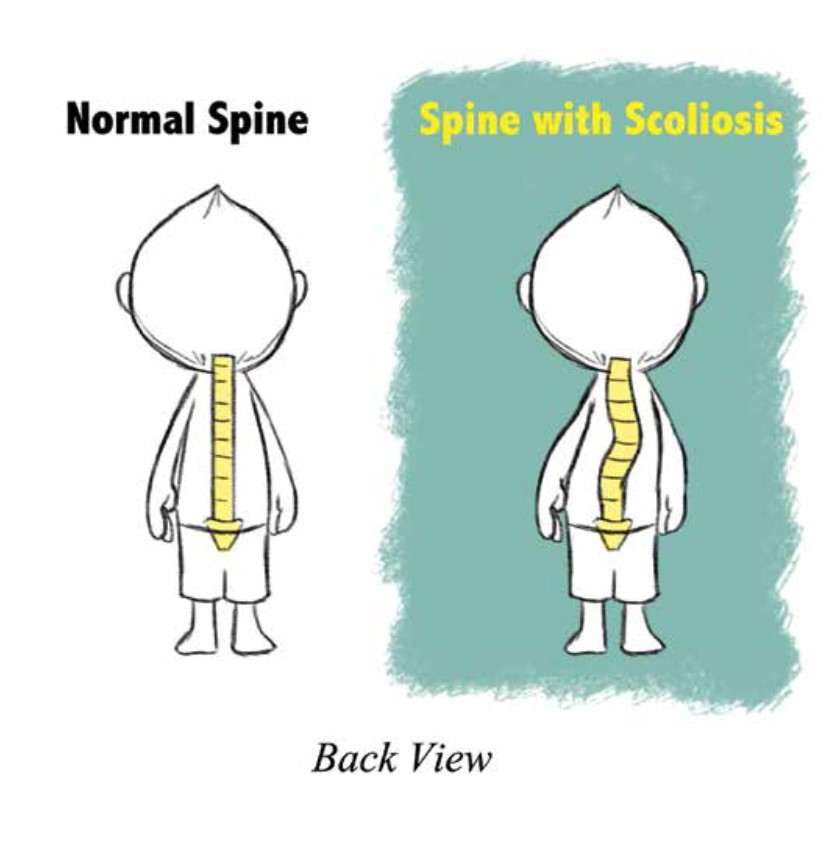
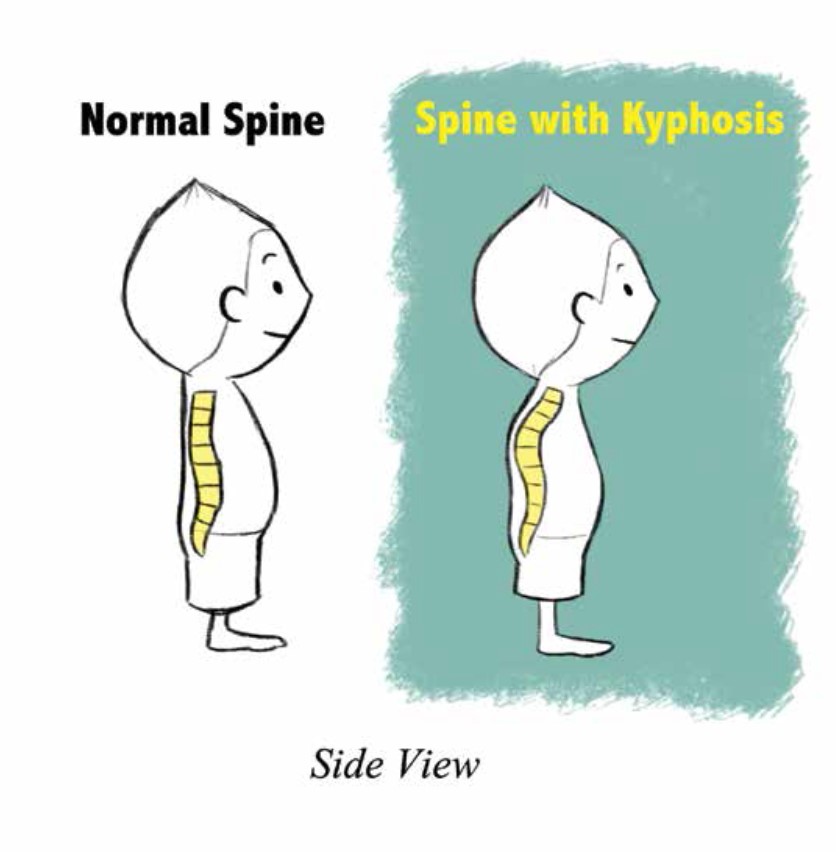
Scoliosis is a curvature of the spine to either side, which is more than 10 degrees. It can also mean an increased kyphosis, which is an over-curvature of the upper portion of the back. 2-3% of the U.S. population has a form of scoliosis. Early onset scoliosis (EOS) is a scoliosis identified or diagnosed by a doctor in patients under the age of 10.
There are several types of EOS: some is caused by misshaped bones (vertebra) in the spine, this is called congenital; some patients have a neuromuscular disease like muscular dystrophy where the muscles cannot hold the spine straight; other patients have a diagnosed syndrome (a disease with effects on more than one part of the body) that causes scoliosis; and a very small number of patients have EOS with no identified reason and are called idiopathic .
A small number of patients have genetic or inherited EOS (idiopathic, some syndromes), meaning one or both parents had a gene causing scoliosis that is present in their child. If this is true for your family your doctor will inform you of the details and you may be referred to a doctor who specializes in genetics.
Most types of EOS have a known cause (misshaped bones in the spine, or muscular problems such as muscular dystrophy), however some types of scoliosis have no clear cause and are diagnosed as idiopathic (meaning we do not know what the cause is). Not drinking enough milk or wearing a heavy backpack does not cause EOS.
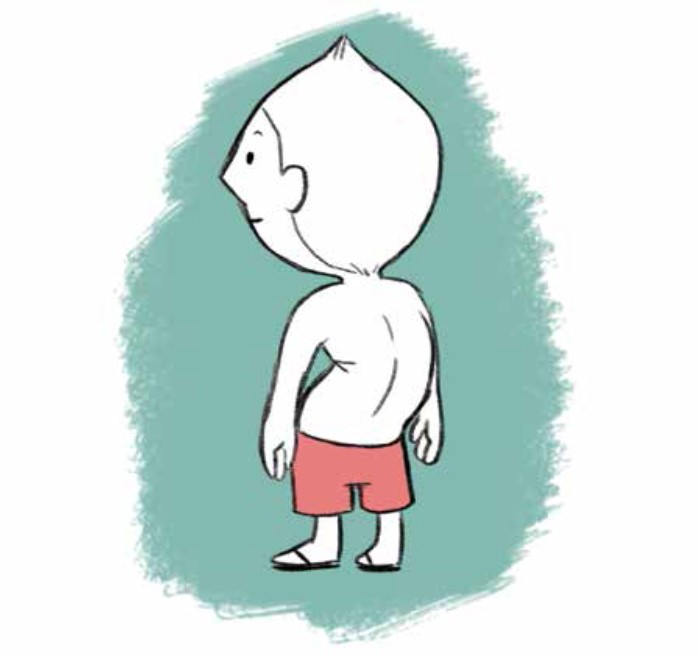
EOS may be picked up when you or someone else may notice your child’s back is curved. Some children with EOS have uneven waists, shoulders and/or shoulder blades, and a “hump” where the ribs stick out more on one side than the other. Sometimes the scoliosis is noticed when a child goes to the doctor for something else (like pneumonia or RSV) and an x-ray of the chest is done.
A pediatrician, pediatric orthopedist and/or spine surgeon can diagnose the scoliosis. Doctors use an x-ray of your child’s spine to confirm the diagnosis. If your doctor finds that your child has EOS, he/she may recommend additional testing and refer your child to other medical specialists.
Patients with mild to moderate scoliosis do not have more back pain than people without scoliosis; however, scoliosis that is severe or caused by an abnormality in the spinal cord can cause back pain.
Your doctor may or may not recommend avoiding contact sports such as football; otherwise a child with scoliosis is usually treated no differently than one who does not have scoliosis.
Tests
The most common test doctors use are x-rays of the spine: one view is back to front and a second view is from the side, these images are used to see how many curves are there and what size they are . Your doctor may also get a special view of the spinal cord or the lungs on an MRI (Magnetic Resonance Imaging) machine. A MRI study of the spine takes around an hour to obtain and a patient has to lie very still the whole time, for young patients this test is usually done under general anesthesia. Testing may also be done using a CT (Computed Tomography) scan to give more detail of how the spine looks in very severe scoliosis. During treatment your child may also have testing to show how well they are breathing, this can be examined by a fingerprick blood test, a pulmonary function test (PFT) where a patient breathes in and out into a machine, and counting the number of breaths in a minute.
Treatment
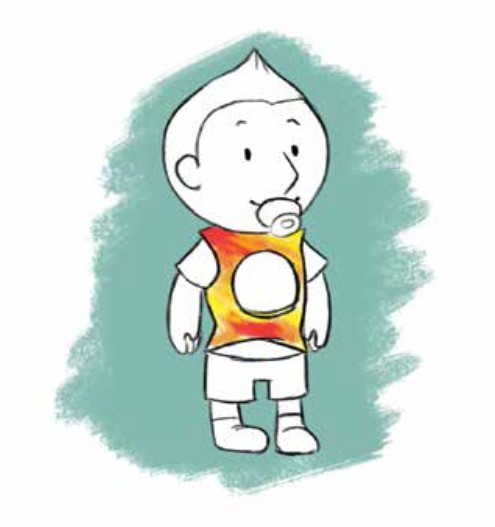
There is a wide range of treatments for EOS, and each patient’s treatment is unique to the child and their doctor. Some patients may only need to be checked during times when the child is rapidly growing. Patients with small to moderate size curves may wear a plastic body brace. Young patients with flexible curves may be put into a series of molded casts. Braces and casts are normally used to prevent the curve from getting worse and are very effective in some patients.
Patients with more severe curves may require surgical correction of their scoliosis. There are several surgical options that allow the spine to grow while controlling the curve; these options include Traditional Growing Rods (TGR), Magnetically Controlled Growing Rods (MAGEC™), Vertical Expandable Prosthetic Titanium Rib (VEPTR®), Growth Guided Devices (Shilla® or Luque Trolley), Tension-based devices (Tether or Staples) or a spinal fusion. Some patients may need to be treated with halo gravity traction in preparation for their surgery.
Some children never need surgery and may simply be observed, or treated with a brace or body casting. Unfortunately there is no way to predict this for any patient.
Observation
Most patients see the doctor 2-4 times a year, however it can range from once a year to monthly visits. Your doctor will decide whether an x-ray is needed each time, but if your child is not in an active growth cycle and the curve has not gotten bigger, an x-ray may not be needed with every visit.
Bracing
Most braces are custom made for the patient. A plaster or foam copy of the patient’s body is made and the brace is made specifically for their body and curve. Some braces are soft and ready made and fitted by straps to the patient.
The more your child wears the brace the better it works - most doctors ask that families try to keep the brace on 18 to 22 hours a day. However it is ok for the brace to come off for organized activities where wearing it would interfere (gymnastics, swimming, soccer, music lessons etc.…).

A brace will not correct or cure scoliosis. When worn most of a 24-hour day, a brace can slow down the growth of a curve. The purpose of a brace is to prevent scoliosis from rapidly worsening in a patient and delaying, or at best, avoiding surgery.
It can take some time to get used to the brace, your doctor and the person who made the brace can help with this. It is very important that if your child is not wearing the brace for more than a few days that you contact your doctor and let them know. Your child’s doctor understands the challenge of brace wear in this age group; you should be able to discuss these challenges with them openly.
Body Casting
Each cast is custom made specifically to the patient’s body and curve. The patient is asleep under general anesthesia and the doctor decreases the curve and then holds it in place with the cast.
Body casts are not removable and are designed to be on the patient 24/7. Your doctor will give you instructions on keeping your child clean while in the cast.

Casts are usually in a series and can be from 2 to 5 or more, each cast can be in place from 3 weeks to 12 weeks. The number of casts needed and how long each cast is worn will be decided by your doctor based on how the scoliosis changes in each cast.
If your child is under the age of three and does not have a severe curve, it is possible that the casts will completely correct or cure the scoliosis. If your child is over the age of three and/or has a severe curve, the goal of casting is often to delay surgery. Your child’s specific case and the goals for casting will be discussed by your doctor.
Cast vacations will vary by patient and doctor. Many patients will take a planned break during the summer, or for some other planned activity (vacation at a water park or beach).
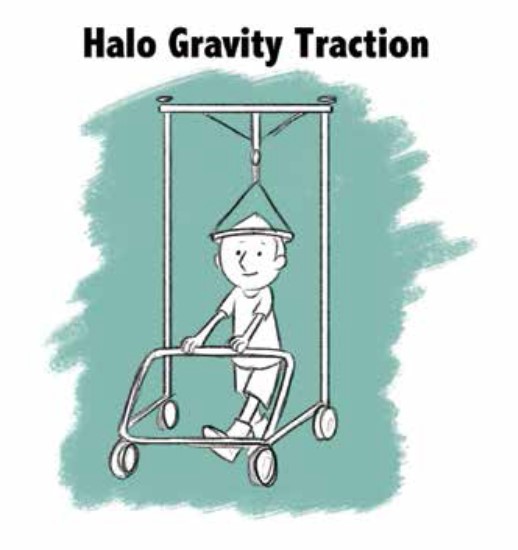
Halo Gravity Traction
The goals of halo gravity traction are:
- Gradually and safely make a curve smaller
- Make it easier for a patient to breathe effectively
- Help a patient gain weight and improve nutrition
- Prepare the spinal cord for correction of the scoliosis.
This is placed in the operating room. While the patient is asleep under general anesthesia, several pins attach the halo ring to the patient’s skull. The next day the halo ring is attached to a walker or wheelchair and a small amount of weight (a few pounds) pulls the patient’s body upward. As the patient is comfortable with the weight, a little more is added each day or so until the maximum amount is reached (usually somewhere close to half the patient’s body weight).
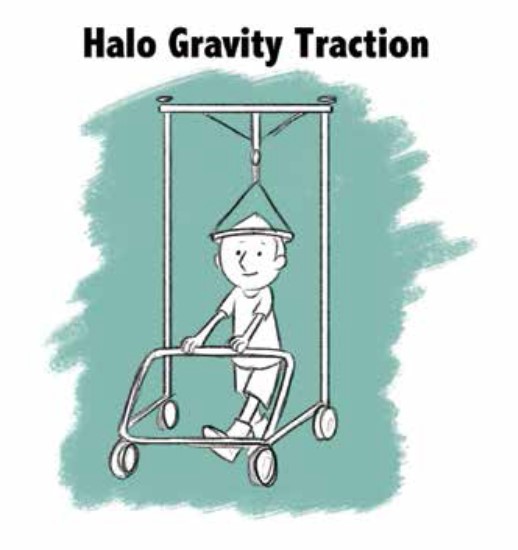
Patients may have a headache the first day or two, otherwise it is not painful. In fact, many patients feel more comfortable once in traction, as breathing and eating can be easier.
Complications such as nerve damage are rare. Hospital staff will teach the family how to check for any nerve damage on a regular basis, and what to do if they see any.
Patients may be in traction for 4 weeks and up to 12 weeks typically. There is special equipment that attaches to the bed frame and allows the patient to be in traction while sleeping.
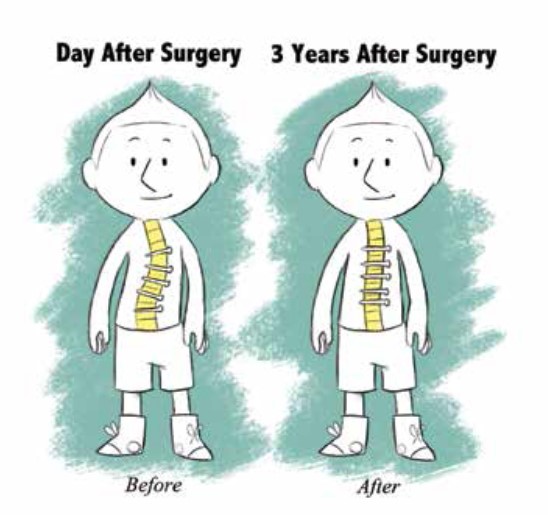
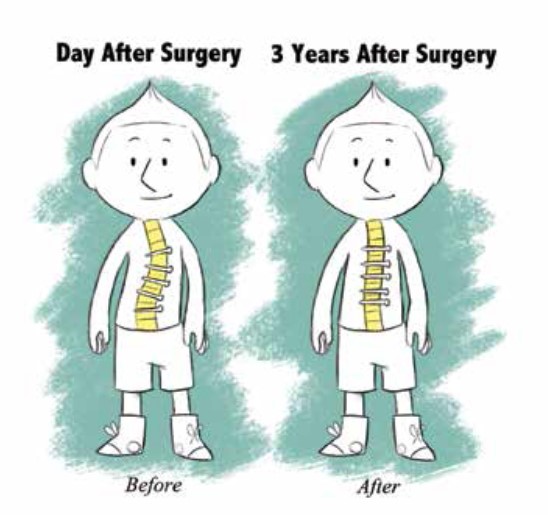
Surgery
The length of time in the hospital after surgery depends on the type of the surgery and the health of the patient. For the very first or initial surgery most patients will stay for 2-5 days. For patients with a device that is lengthened during a surgery a 1-2 day stay may be required but they may be able to go home the same day. For patients with a device that is lengthened magnetically they can go home the same day.
Some patients may need to wear a brace for 3 to 6 months after the very first surgery. This is to make sure that the bone heals around the spinal anchors. For devices that are lengthened, patients are not typically braced for lengthening procedures.
The first surgery it can take from 2-6 hours depending on the patient’s spine and general health.
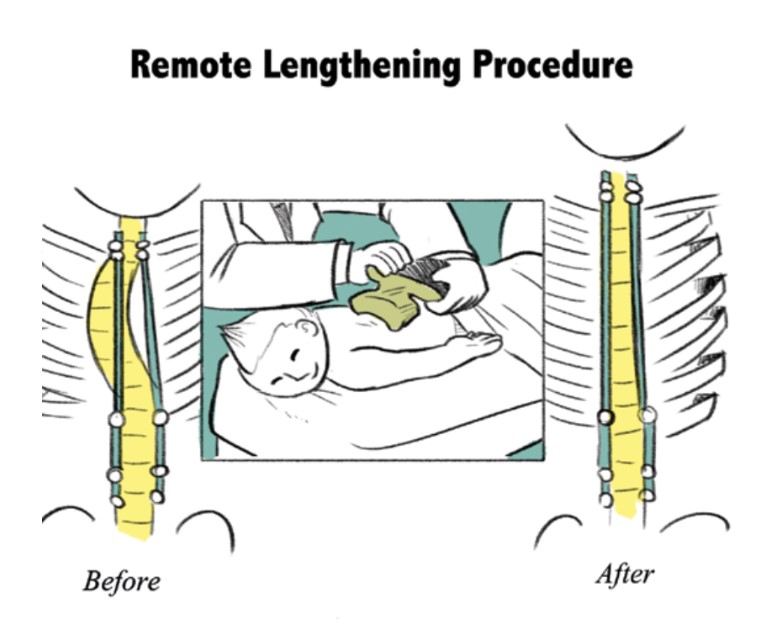
For surgical lengthenings (on devices like Growing Rods and VEPTR®) without complications, surgery with general anesthesia usually takes about 1 hour.
At the very first, or initial, surgery, we encourage our families to limit the patient to mild forms of exercise (walking, running, calm play with other children) for the 4-12 weeks after surgery. When your doctor advises they can return to normal activities outside of contact sports (football). However, this may vary by patient and doctor, so please ask your doctor for specific instructions for your child.
Complications
Surgery for EOS can be challenging to treat effectively and safely due to the age and size of patients. Minor complications like slow or poor healing of the wound, or anchors that move or break can occur but they usually be corrected with minimal treatment. Major complications can include injury to the spinal cord, deep infection in the area of surgery, and failure of the first surgery to control the scoliosis. These complications are less common but do need more intensive treatment. Every effort is taken to avoid all of the above, but complications can and do occur, so you should discuss the risks for your child with their doctor.
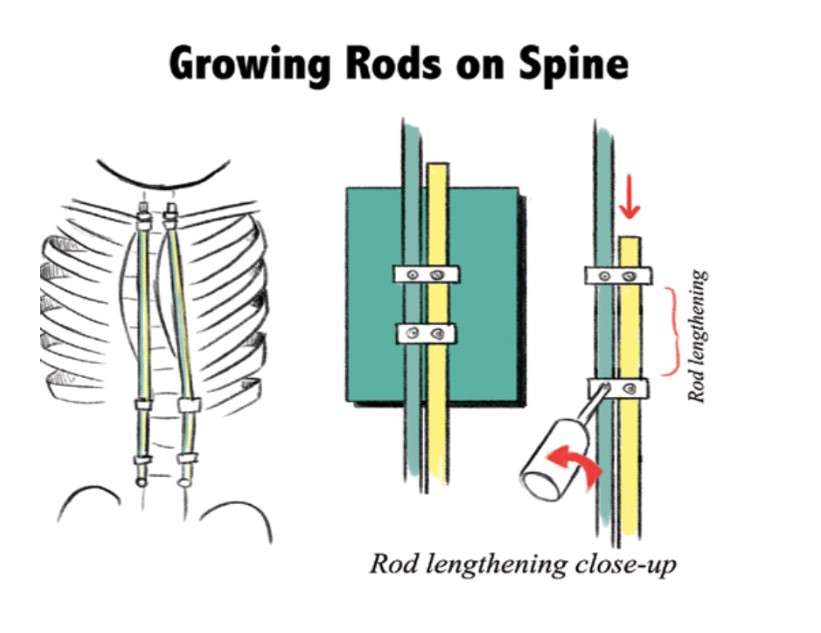
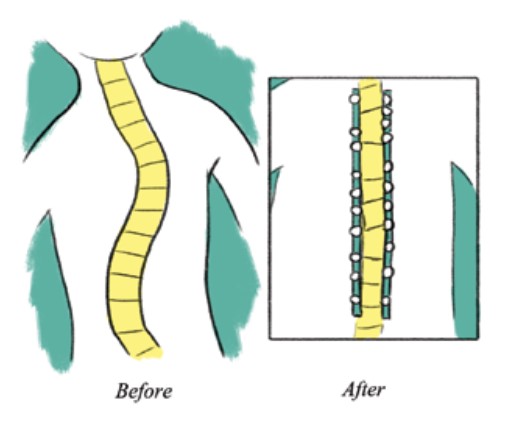
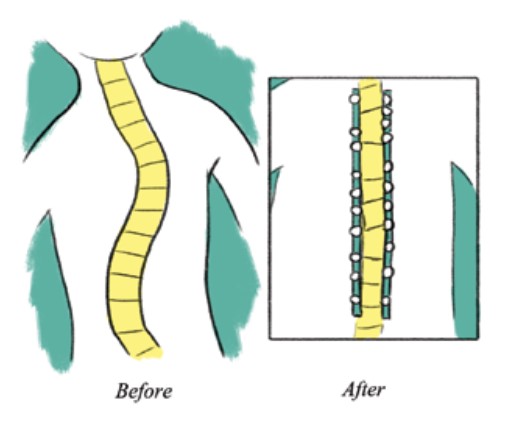
Growing Rods
Growing Rods are two rods on either side of the spine 16 attached to the spinal vertebrae above and below a curve with spine anchors (hooks, screws or wires). The anchors and rods are used to correct some of the scoliosis and help the spine grow straighter and longer. The rods are extendable to make them longer as a child grows, using a child’s natural periods of growth to both straighten and lengthen the spine over time.
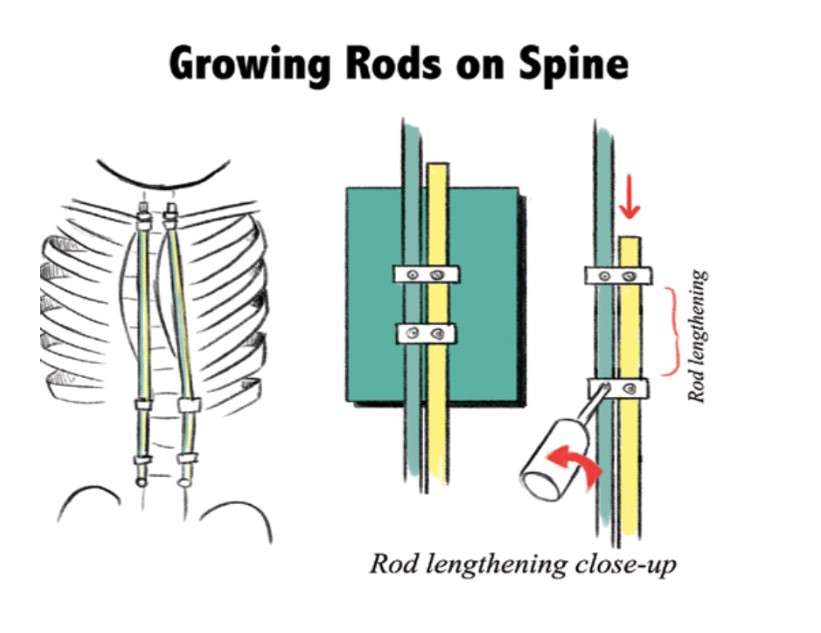
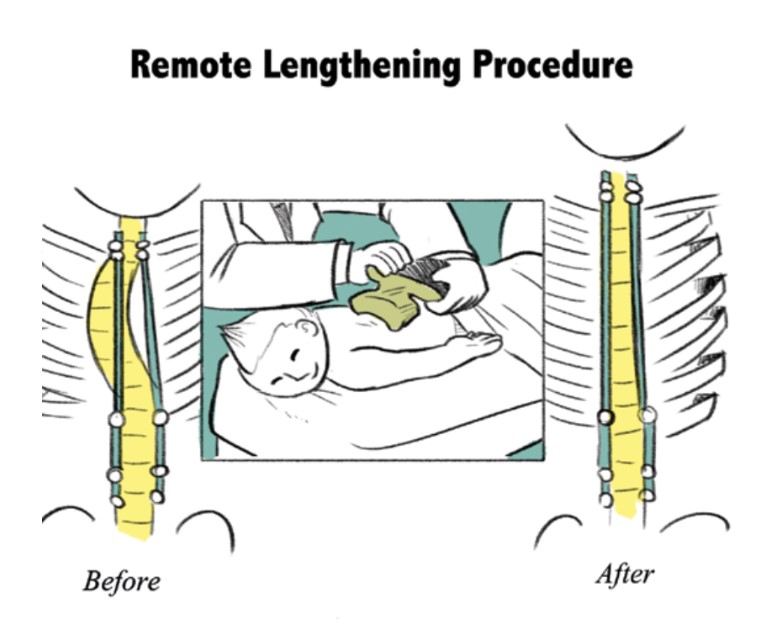
Growing Rods may be either traditional (requiring a small surgical incision for manual lengthening under general anesthesia) or magnetic (no incision is required for the lengthening procedures) where a medical magnet is placed on the skin over the spine by the doctor to lengthen the rod(s) in the doctor’s office with the child awake.
Frequency of lengthenings will vary by patient and doctor; most patients will have an average of 2 lengthenings a year. Once a patient is close to the end of spinal growth, the doctor will discuss options.
MAGEC is a magnetically controlled growing rod that after the first surgery can be lengthened with an external set of strong magnets without surgery. The system has been approved by the FDA and examined in both animals and humans and shown to be safe and effective. Your child can now undergo the MCGR (Magnetically Controlled Growing Rod) procedure in the United States.
Frequency of lengthenings will vary by patient and doctor; most patients can have an average of 4-12 lengthenings a year. Once a patient is close to the end of spinal growth, the doctor will discuss options, which may include a final surgery to correct any remaining scoliosis, or no further surgery at all.
While there is no acute pain felt with the lengthening, patients may feel some anxiety and mild discomfort during a magnetic lengthening.
The lengthening device your doctor uses to extend the rods contains medical grade magnets that are much stronger than those used in public spaces or in the home.
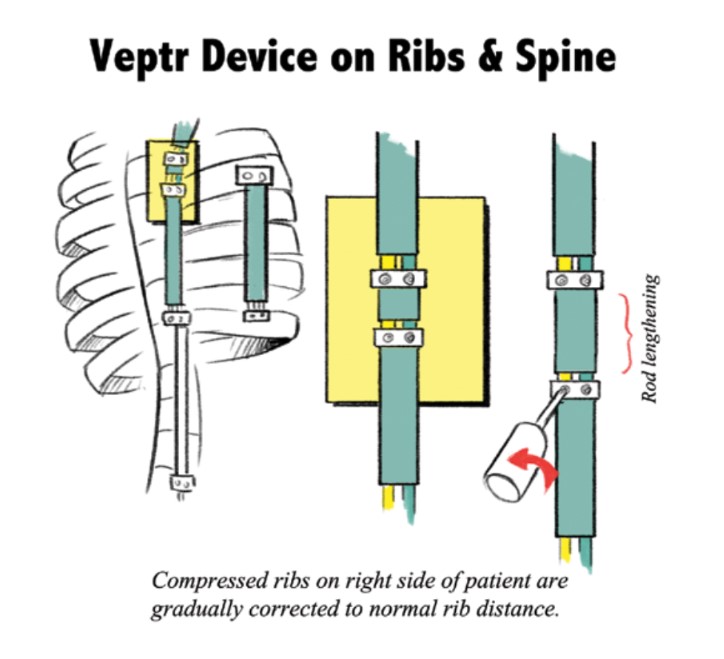
VEPTR® (Vertical Expandable Prosthetic Titanium Rib)
VEPTR® can be one or more curved bars that can attach to the ribs or spine by anchors (clamps, hooks, or screws) 1above and below a curve. The anchors and bars are used to correct some of the scoliosis and help the spine grow straighter and longer and they can be used to treat chest and rib abnormalities that are found in some types of scoliosis. The bars are extendable to make them longer as a child grows, using a child’s natural periods of growth to both straighten and lengthen the spine.
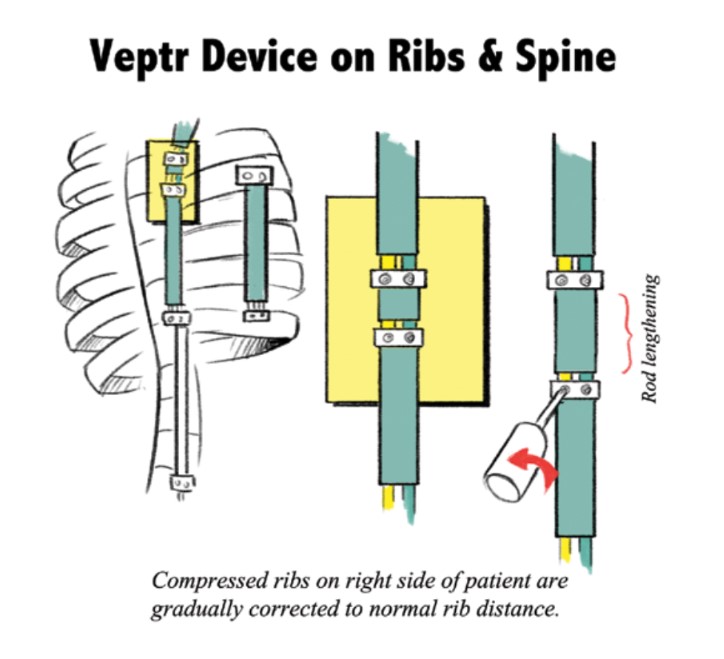
Frequency of lengthenings will vary by patient and doctor; most patients will have an average of 2 lengthenings a year. Once a patient is close to the end of spinal growth, the doctor will discuss options, which may include a final surgery to correct any remaining scoliosis, or no further surgery at all.
Definitive Spinal Fusion
Definitive spinal fusion is when a curve in the spine has been corrected and will not grow any more. In EOS, definitive fusions are usually part of the treatment for patients with congenital curves where normal growth would not happen if left alone. Definitive spinal fusion in congenital patients is usually a small part of the patient’s total spine. Definitive fusion may also be used along with a growing rod to help control a severe scoliosis; again this would be a small part of the patient’s total spine. Most patients will require a definitive fusion at the end of their treatment for EOS if they have been treated with growing rods, VEPTR® or other devices.
In some patients the definitive fusion may be the only surgery they ever need, but this will vary by patient and curve. Your doctor will discuss your child’s case specifically.
Growth Guided Devices (Shilla® or Luque Trolley)
Growth guided devices have fixed anchor points (screws) at the top, middle and bottom of the spine, two rods are attached to the anchors but adjust to the spine’s height as the patient grows. The anchors and rods make a scoliosis smaller while making the spine taller.
Growth guided device patients only have one surgery to place the device and no further surgery is needed unless there are complications or the patient has reached the end of spinal growth and needs a final surgery.
The two most common devices are the Shilla and Luque Trolley devices.
Tension Based Devices (Tether or Vertebral Body Stapling)
(As of June 2016, vertebral body tethers and staples have not been cleared/approved by the U.S. Food and Drug Administration for the treatment of scoliosis.)
Tension based devices have fixed anchor points (screws or staples) along the curve on the convex side; as the child grows the anchors straighten the side of the spine. The anchors make a scoliosis smaller while making the spine taller as the patient grows.
Tension based device patients only have one surgery to place the device and may need a second to remove part of the device when a curve is corrected. No further surgery is needed unless there are complications or the patient has reached the end of spinal growth and needs a final surgery.
The two most common devices are the Tether and Vertebral Body Stapling devices.
Learn More
Condition QR Code:

What is Early-Onset Scoliosis?
Scoliosis is a curvature of the spine to either side, which is more than 10 degrees. It can also mean an increased kyphosis, which is an over-curvature of the upper portion of the back. 2-3% of the U.S. population has a form of scoliosis. Early onset scoliosis (EOS) is a scoliosis identified or diagnosed by a doctor in patients under the age of 10.
Is all EOS the same?
No, there are several types of EOS: some is caused by misshaped bones (vertebra) in the spine, this is called congenital; some patients have a neuromuscular disease like muscular dystrophy where the muscles cannot hold the spine straight; other patients have a diagnosed syndrome (a disease with effects on more than one part of the body) that causes scoliosis; and a very small number of patients have EOS with no identified reason and are called idiopathic.
Is scoliosis passed on to the child by parents or relatives?
A small number of patients have genetic or inherited EOS (idiopathic, some syndromes), meaning one or both parents had a gene causing scoliosis that is present in their child. If this is true for your family your doctor will inform you of the details and you may be referred to a doctor who specializes in genetics.
What Causes EOS?
Most types of EOS have a known cause (misshaped bones in the spine, or muscular problems such as muscular dystrophy), however some types of scoliosis have no clear cause and are diagnosed as idiopathic (meaning we do not know what the cause is). Not drinking enough milk or wearing a heavy backpack does not cause EOS.
How is EOS noticed in most children?
You or someone else may notice your child’s back is curved. Some children with EOS have uneven waists, shoulders and/or shoulder blades, and a “hump” where the ribs stick out more on one side than the other. Sometimes the scoliosis is noticed when a child goes to the doctor for something else (like pneumonia or RSV) and an x-ray of the chest is done.
How does a doctor diagnose EOS?
A pediatrician, pediatric orthopedist and/or spine surgeon can diagnose the scoliosis. Doctors use an x-ray of your child’s spine to confirm the diagnosis. If your doctor finds that your child has EOS, he/she may recommend additional testing and refer your child to other medical specialists.
Does scoliosis hurt?
Patients with mild to moderate scoliosis do not have more back pain than people without scoliosis; however, scoliosis that is severe or caused by an abnormality in the spinal cord can cause back pain.
How do I know if the curve will get bigger?
This will depend on the type of scoliosis your child has, as well as how old they are. Your doctor will discuss the specifics with you. If you notice a big change in their back, you need to notify your doctor.
Should I limit my child’s activities?
Your doctor may or may not recommend avoiding contact sports such as football; otherwise a child with scoliosis is usually treated no differently than one who does not have scoliosis.
What complications can my child have?
Severe scoliosis may make it harder for your child to breathe, which in turn may make it hard for them to gain weight and grow and develop in general. Certain types of spine deformities that are more noticeable from a side view (kyphosis) may pinch the spinal cord causing neurologic symptoms such as pain, numbness or weakness.
What kind of medical tests will be done for my child?
The most common test doctors use are x-rays of the spine: one view is back to front and a second view is from the side, these images are used to see how many curves are there and what size they are . Your doctor may also get a special view of the spinal cord or the lungs on an MRI (Magnetic Resonance Imaging) machine. A MRI study of the spine takes around an hour to obtain and a patient has to lie very still the whole time, for young patients this test is usually done under general anesthesia. Testing may also be done using a CT (Computed Tomography) scan to give more detail of how the spine looks in very severe scoliosis. During treatment your child may also have testing to show how well they are breathing, this can be examined by a fingerprick blood test, a pulmonary function test (PFT) where a patient breathes in and out into a machine, and counting the number of breaths in a minute.
Do I need to worry about the number of x-rays and imaging studies my child is getting?
Your doctor will limit the number and type of x-rays and imaging needed to what is necessary to treat your child. While the amount of radiation at a young age is a concern, the greater problem is being able to properly “see” the scoliosis and how it is responding to treatment. Newer types of x-ray machines, like EOS imaging, are being invented to reduce the amount of radiation when getting x-rays of a patient.
What are the treatment options for EOS?
There is a wide range of treatments for EOS, and each patient’s treatment is unique to the child and their doctor. Some patients may only need to be checked during times when the child is rapidly growing. Patients with small to moderate size curves may wear a plastic body brace. Young patients with flexible curves may be put into a series of molded casts. Braces and casts are normally used to prevent the curve from getting worse and are very effective in some patients.
Patients with more severe curves may require surgical correction of their scoliosis. There are several surgical options that allow the spine to grow while controlling the curve; these options include Traditional Growing Rods (TGR), Magnetically Controlled Growing Rods (MAGEC™), Vertical Expandable Prosthetic Titanium Rib (VEPTR®), Growth Guided Devices (Shilla® or Luque Trolley), Tension-based devices (Tether or Staples) or a spinal fusion. Some patients may need to be treated with halo gravity traction in preparation for their surgery.
Can my child totally avoid surgery?
Some children never need surgery and may simply be observed, or treated with a brace or body casting. Unfortunately there is no way to predict this for any patient.
Observation
How often will we see the doctor?
Ultimately this will depend on your child’s age, type of scoliosis, treatment being used, and where they are in their growth cycle. Most patients see the doctor 2-4 times a year, however it can range from once a year to monthly visits.
Do we need an x-ray every time?
Your doctor will make this decision, but if your child is not in an active growth cycle and the curve has not gotten bigger, an x-ray may not be needed with every visit.
Bracing
How is the brace made?
Most braces are custom made for the patient. A plaster or foam copy of the patient’s body is made and the brace is made specifically for their body and curve. Some braces are soft and ready made and fitted by straps to the patient.
How much does my child have to wear the brace?
The more your child wears the brace the better it works - most doctors ask that families try to keep the brace on 18 to 22 hours a day. However it is ok for the brace to come off for organized activities where wearing it would interfere (gymnastics, swimming, soccer, music lessons etc.…).
Will the brace “cure” the scoliosis?
A brace will not correct or cure scoliosis. When worn most of a 24-hour day, a brace can slow down the growth of a curve. The purpose of a brace is to prevent scoliosis from rapidly worsening in a patient and delaying, or at best, avoiding surgery.
What if my child can’t or won’t wear the brace?
It is very important that if your child is not wearing the brace for more than a few days that you contact your doctor and let them know. It can take some time to get used to the brace, your doctor and the person who made the brace can help with this. Your child’s doctor understands the challenge of brace wear in this age group; you should be able to discuss these challenges with them openly.
Can we take a break or vacation from the brace?
This will vary by patient and doctor, but most patients may take the brace off to swim, or for some other planned activity (gymnastics, party, water sports) for a short period of time.
Body Casting
How is the cast made?
Each cast is custom made specifically to the patient’s body and curve. The patient is asleep under general anesthesia and the doctor decreases the curve and then holds it in place with the cast.
Can the cast come off?
Body casts are not removable and are designed to be on the patient 24/7. Your doctor will give you instructions on keeping your child clean while in the cast.
How many casts will my child have? And how long is each cast on?
Casts are usually in a series and can be from 2 to 5 or more, each cast can be in place from 3 weeks to 12 weeks. The number of casts needed and how long each cast is worn will be decided by your doctor based on how the scoliosis changes in each cast.
Will the cast “cure” the scoliosis?
If your child is under the age of three and does not have a severe curve, it is possible that the casts will completely correct or cure the scoliosis. If your child is over the age of three and/or has a severe curve, the goal of casting is often to delay surgery. Your child’s specific case and the goals for casting will be discussed by your doctor.
What if my child breaks the cast?
It is very important that if your child’s cast is broken that you contact your doctor and let them know as soon as possible.
Can we take a break or vacation from the cast?
This will vary by patient and doctor. Many patients will take a planned break during the summer, or for some other planned activity (vacation at a water park or beach).
Halo Gravity Traction
What does halo gravity traction do?
The goals of halo gravity traction are:
- Gradually and safely make a curve smaller
- Make it easier for a patient to breathe effectively
- Help a patient gain weight and improve nutrition
- Prepare the spinal cord for correction of the scoliosis.
How does halo gravity traction work?
While the patient is asleep under general anesthesia, several pins attach the halo ring to the patient’s skull. The next day the halo ring is attached to a walker or wheelchair and a small amount of weight (a few pounds) pulls the patient’s body upward. As the patient is comfortable with the weight, a little more is added each day or so until the maximum amount is reached (usually somewhere close to half the patient’s body weight).
Is halo gravity traction painful?
Patients may have a headache the first day or two, otherwise it is not painful. In fact, many patients feel more comfortable once in traction, as breathing and eating can be easier.
Is halo gravity traction dangerous?
There can be nerve damage, but this is rare. Hospital staff will teach the family how to check for any nerve damage on a regular basis, and what to do if they see any.
How long will my child be in halo gravity traction?
This will depend on how the curve and your child react to the halo gravity traction; patients may be in traction for 4 weeks and up to 12 weeks typically.
How do patients sleep in halo gravity traction?
There is special equipment that attaches to the bed frame and allows the patient to be in traction while sleeping.
Surgery
How long should my child stay at hospital after surgery?
It depends on the type of the surgery and the health of the patient. For the very first or initial surgery most patients will stay for 2-5 days. For patients with a device that is lengthened during a surgery a 1-2 day stay may be required but they may be able to go home the same day. For patients with a device that is lengthened magnetically they can go home the same day.
Does my child need to wear brace after surgery?
Some patients may need to wear a brace for 3 to 6 months after the very first surgery. This is to make sure that the bone heals around the spinal anchors. For devices that are lengthened, patients are not typically braced for lengthening procedures.
How long does the surgery take?
For the first surgery it can take from 2-6 hours depending on the patient’s spine and general health. For surgical lengthenings (on devices like Growing Rods and VEPTR®) without complications, surgery with general anesthesia usually takes about 1 hour.
Will my child have some limitations in sports or physical activities after surgery?
At the very first, or initial, surgery, we encourage our families to limit the patient to mild forms of exercise (walking, running, calm play with other children) for the 4-12 weeks after surgery. When your doctor advises they can return to normal activities outside of contact sports (football). However, this may vary by patient and doctor, so please ask your doctor for specific instructions for your child.
What are the complications that can happen?
Surgery for EOS can be challenging to treat effectively and safely due to the age and size of patients. Minor complications like slow or poor healing of the wound, or anchors that move or break can occur but they usually be corrected with minimal treatment. Major complications can include injury to the spinal cord, deep infection in the area of surgery, and failure of the first surgery to control the scoliosis. These complications are less common but do need more intensive treatment. Every effort is taken to avoid all of the above, but complications can and do occur, so you should discuss the risks for your child with their doctor.
When will my child’s treatment end?
The course of treatment for each patient is different and depends on several factors including: age at initial surgery, the cause of scoliosis, what surgical method is used, how much growth their spine has and the number and type of complications; your doctor will discuss the specifics with you.
Growing Rods
What are Growing Rods and how do they work?
Growing Rods are two rods on either side of the spine 16 attached to the spinal vertebrae above and below a curve with spine anchors (hooks, screws or wires). The anchors and rods are used to correct some of the scoliosis and help the spine grow straighter and longer. The rods are extendable to make them longer as a child grows, using a child’s natural periods of growth to both straighten and lengthen the spine over time.
Is there more than one type of Growing Rod system?
Growing Rods may be either traditional (requiring a small surgical incision for manual lengthening under general anesthesia) or magnetic (no incision is required for the lengthening procedures) where a medical magnet is placed on the skin over the spine by the doctor to lengthen the rod(s) in the doctor’s office with the child awake.
How often and for how long will my child have multiple surgeries (lengthenings) for traditional growing rods?
Frequency of lengthenings will vary by patient and doctor; most patients will have an average of 2 lengthenings a year. Once a patient is close to the end of spinal growth, the doctor will discuss options, which may include a final surgery to correct any leftover scoliosis, or no further surgery at all.
What is the MAGEC device and MCGR procedure? Can my child undergo this treatment in United States?
MAGEC is a magnetically controlled growing rod that after the first surgery can be lengthened with an external set of strong magnets without surgery. The system has been approved by the FDA and examined in both animals and humans and shown to be safe and effective. Your child can now undergo the MCGR (Magnetically Controlled Growing Rod) procedure in the United States.
How often and for how long will my child have multiple magnetic lengthenings?
Frequency of lengthenings will vary by patient and doctor; most patients can have an average of 4-12 lengthenings a year. Once a patient is close to the end of spinal growth, the doctor will discuss options, which may include a final surgery to correct any remaining scoliosis, or no further surgery at all.
Does the MCGR lengthening hurt?
While there is no acute pain felt with the lengthening, patients may feel some anxiety and mild discomfort during a magnetic lengthening.
Do we need to avoid magnets in public or at home?
The lengthening device your doctor uses to extend the rods contains medical grade magnets that are much stronger than those used in public spaces or in the home.
VEPTR® (Vertical Expandable Prosthetic Titanium Rib)
What is a VEPTR® and how does it work?
VEPTR® can be one or more curved bars that can attach to the ribs or spine by anchors (clamps, hooks, or screws) 1above and below a curve. The anchors and bars are used to correct some of the scoliosis and help the spine grow straighter and longer and they can be used to treat chest and rib abnormalities that are found in some types of scoliosis. The bars are extendable to make them longer as a child grows, using a child’s natural periods of growth to both straighten and lengthen the spine.
How often and for how long will my child have multiple surgeries (lengthenings)?
Frequency of lengthenings will vary by patient and doctor; most patients will have an average of 2 lengthenings a year. Once a patient is close to the end of spinal growth, the doctor will discuss options, which may include a final surgery to correct any remaining scoliosis, or no further surgery at all.
Definitive Spinal Fusion
What is a definitive spinal fusion and how does it work in EOS?
Definitive spinal fusion is when a curve in the spine has been corrected and will not grow any more. In EOS, definitive fusions are usually part of the treatment for patients with congenital curves where normal growth would not happen if left alone. Definitive spinal fusion in congenital patients is usually a small part of the patient’s total spine 19 . Definitive fusion may also be used along with a growing rod to help control a severe scoliosis 20 ; again this would be a small part of the patient’s total spine. 21 Most patients will require a definitive fusion at the end of their treatment for EOS if they have been treated with growing rods, VEPTR® or other devices.
If my child has a definitive fusion does that mean they will never need another surgery?
In some patients the definitive fusion may be the only surgery they ever need, but this will vary by patient and curve. Your doctor will discuss your child’s case specifically.
Growth Guided Devices (Shilla® or Luque Trolley)
What is a growth guided device and how does it work?
Growth guided devices have fixed anchor points (screws) at the top, middle and bottom of the spine, two rods are attached to the anchors but adjust to the spine’s height as the patient grows. The anchors and rods make a scoliosis smaller while making the spine taller.
Does the device need more than one surgery?
Growth guided device patients only have one surgery to place the device and no further surgery is needed unless there are complications or the patient has reached the end of spinal growth and needs a final surgery.
Are there different types of growth guided devices?
Yes, the two most common devices are the Shilla and Luque Trolley devices.
Tension Based Devices (Tether or Vertebral Body Stapling)
(As of June 2016, vertebral body tethers and staples have not been cleared/approved by the U.S. Food and Drug Administration for the treatment of scoliosis.)
What is a tension based device and how does it work?
Tension based devices have fixed anchor points (screws or staples) along the curve on the convex side; as the child grows the anchors straighten the side of the spine. The anchors make a scoliosis smaller while making the spine taller as the patient grows.
Does the tension based device need more than one surgery?
Tension based device patients only have one surgery to place the device and may need a second to remove part of the device when a curve is corrected. No further surgery is needed unless there are complications or the patient has reached the end of spinal growth and needs a final surgery.
Are there different types of tension based devices?
Yes the two most common devices are the Tether and Vertebral Body Stapling devices.

 POSNA.org
POSNA.org